Anxiety & The Breath
Breathing and Anxiety: Exploring the Science of Respiration and Fear
Introduction
“Take a deep breath” is often what we tell someone who is anxious. We intuitively recognise the link between between and our fear. Anxiety, changes in breathing: rapid chest breathing, sighs, or even the feeling of being unable to catch one’s breath. Conversely, controlled breathing practices are a cornerstone of many relaxation and stress-management techniques. The autonomic nervous system is component of the peripheral nervous system that regulates involuntary physiologic processes including heart rate, blood pressure, respiration, digestion, and sexual arousal. It contains three anatomically distinct divisions: sympathetic, parasympathetic, and enteric. During anxiety our sympathetic nervous system becomes dominant as our body prepares us to fight-or-flight.
Anxiety is when this becomes chronic. Defined as: “any of a group of mental conditions characterized by excessive fear of or apprehension about real or perceived threats, leading to altered behavior and often to physical symptoms such as increased heart rate or muscle tension.” Anxiety effects 30% of the worlds population at some point in their lives and 4% of the worlds population at any given time. What is it about the breath that so profoundly influences anxiety? Well, our breath is one of the few ways we have to influence the autonomic nervous system consciously. This article delves into the relationship between breathing and anxiety states, examining the physiological and psychological mechanisms that connect them, how disordered breathing features in anxiety disorders like panic disorder, generalized anxiety disorder (GAD), and post-traumatic stress disorder (PTSD), and how breathing-based interventions can be used.
Mechanisms Linking Breathing and Anxiety
Physiological Pathways: The Breath–Body Connection
Breathing has a direct line to the body’s arousal systems. When we perceive danger (real or imagined), the sympathetic “fight-or-flight” response kicks in, often speeding up respiration to prepare for action. As our brains evolved a long time ago this was more often running from a lion than letting down your unreasonable boss. This can lead to hyperventilation – breathing more rapidly or deeply than needed – which causes a drop in carbon dioxide (CO₂) levels in the blood (hypocapnia). If you had been running from a lion, your muscles would have generated CO₂ that would have offset some of this drop. Hyperventilation has complex effects: it can induce lightheadedness, tingling, or chest tightness, sensations that can further fuel anxiety. Indeed, researchers have found that individuals across a wide range of anxiety disorders tend to hyperventilate both chronically and acutely, indicating that over-breathing is a common feature of pathological anxiety (pubmed.ncbi.nlm.nih.gov). This physiological change isn’t just a side effect of anxiety; it can actively contribute to the anxious state. Over-breathing lowers CO₂ and alters blood pH, which in turn can trigger symptoms (dizziness, faintness, palpitations) that alarm the person and reinforce the fear that something is “wrong,” creating a vicious cycle.
At the same time, the breath offers a gateway to calming the body. Slow, deep breathing (especially engaging the diaphragm) activates the parasympathetic nervous system (the “rest-and-digest” counterpart to fight-or-flight). Deliberate slow breathing increases vagal nerve signals that slow the heart and promote relaxation (pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov). In essence, by slowing our breath we can tilt the autonomic balance toward a calmer state. Research on paced breathing (for example, breathing around 6–10 breaths per minute) shows that it enhances the communication between respiratory and cardiovascular systems, increasing measures like respiratory sinus arrhythmia (the natural variation in heart rate with breathing) and heart rate variability (HRV) that reflect parasympathetic tone (pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov). This physiologically “safety signal” opposes the hyperarousal of anxiety. In short, breathing is a two-way street: anxiety can upset our respiratory rhythms, but by intentionally adjusting our breathing we can send feedback to our brain and body to temper anxiety.
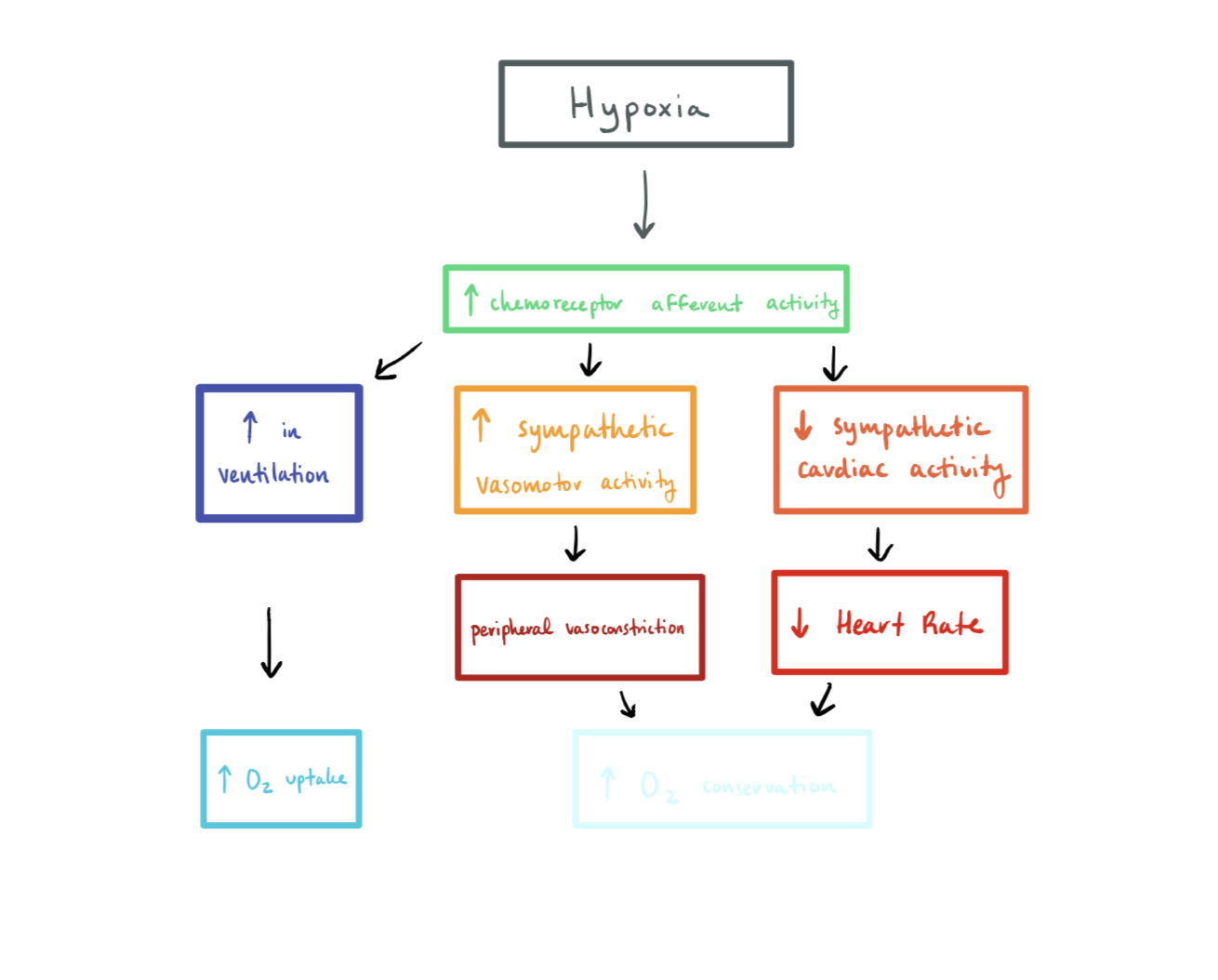
Another key physiological link involves chemoreceptors and the brain’s fear circuitry. The levels of CO₂ and oxygen in our blood are meticulously monitored by the body. Elevated CO₂ (as might occur in suffocating environments or if one holds their breath) is a potent biological stressor – it signals the risk of asphyxiation. The brain’s alarm centers appear highly sensitive to CO₂. Notably, the amygdala (a region central to fear and panic) contains acid-sensing neurons that respond to slight increases in acidity (which accompanies rising CO₂). In a landmark discovery, researchers found that inhaling air high in CO₂ triggers intense fear behaviors in animals, and that this response requires specific acid-sensing ion channels in the amygdala (scientificamerican.com). In other words, the brain is wired to detect when breathing is compromised or CO₂ is accumulating, and to sound an alarm – likely an evolutionary adaptation to push us to escape suffocation. This helps explain why infusing CO₂ or other respiratory stressors can provoke anxiety and panic: the body’s internal monitors are telling the brain “you’re not getting enough air.” In humans, experiments have long shown that breathing air with high CO₂ content (e.g. 35% CO₂) reliably induces anxiety and panic sensations – especially in people prone to panic attacks (scientificamerican.com). Panic disorder patients, in fact, are unusually sensitive to CO₂; most will experience a panic attack when inhaling a CO₂-rich mixture that has little effect on healthy individuals (scientificamerican.com). This hypersensitivity can even be observed in close relatives of panic sufferers, hinting at an inherited component to the CO₂ alarm sensitivity (scientificamerican.com).
Thus, on a physiological level, the breathing–anxiety link is rooted in our basic biology: rapid, shallow breathing and fluctuating CO₂ levels can act as triggers and feedback signals in the anxiety response. Practicing Buteyko Breathing is a way to retrain the bodies chemoreceptors to tolerate higher, more normalized, levels of CO₂. Buteyko breathing empathizes breathing low (using the diaphragm), slow (reducing the respiratory rate), and light (less air to increase CO₂). The Breatheology Method emphasizes that the key to relaxation is exhalation, that our exhalation needs to be longer than our inhalation in order to relax the autonomic nervous system. If you are ready to jump in and learn these methods you can book now with me or continue reading on.
Psychological and Cognitive Factors
While the physiology is critical, the story is not complete without the psychological dimension. Our perception and interpretation of breathing sensations play a huge role in anxiety. Anxiety often heightens interoception – awareness of internal bodily states – but in a biased way: benign fluctuations in heartbeats or breathing can be misread as dangerous. For example, an otherwise harmless shortness of breath can be misinterpreted as “I’m suffocating” or “I might stop breathing,” fueling panic. One influential cognitive model of panic (developed by David Clark in 1986) proposed that panic attacks result from catastrophic misinterpretations of bodily sensations such as changes in breathing or heart rate. If a person believes their slight shortness of breath is a sign of imminent collapse, their anxiety spikes, which in turn further alters breathing, creating a self-perpetuating loop. This model shifted focus to how thoughts about breathing (e.g. “I can’t get air, I will suffocate”) can trigger anxiety even if physiology alone might not (pubmed.ncbi.nlm.nih.gov). Indeed, by the mid-1980s researchers argued that panic and anxiety could best be understood as an interplay between physiological changes and their cognitive appraisal (pubmed.ncbi.nlm.nih.gov). Past experiences, context, and attention all shape this interplay. For instance, a trauma survivor might feel a normal breath hitch and instantly flash back to a life-threatening event, interpreting the sensation as danger in the present. Thereby, we at Breathcraft Lab believe that learning the tools to consciously control your own breathing enable empowerment and personal self efficacy in order for you to take control of your anxiety symptoms.
Anxiety sensitivity – a trait describing how fearful one is of anxiety symptoms themselves – often involves sensitivity to respiratory symptoms. People high in anxiety sensitivity are more likely to react with fear to feelings of breathlessness or a racing heart, believing these sensations are harmful. Thus, the fear of the feeling of not being able to breathe becomes a generator of further anxiety. In disorders like panic disorder and PTSD, this can manifest as a fear of any bodily context that resembles the feared state (such as feeling even mildly winded, which reminds one of panic or of traumatic asphyxiation). Over time, this leads some individuals to develop maladaptive breathing behaviors. For example, someone afraid of panic attacks might start monitoring their breathing very closely and take excessive deep breaths “just in case,” ironically increasing the chance of hyperventilation. Others might do the opposite and breath-hold or suppress normal breaths out of fear of feeling any sensation, leading to irregular breathing patterns. These learned behaviors illustrate how anxiety can condition our breathing habits, and how our beliefs about breathing (e.g. “I must control my breath or something bad will happen”) can maintain anxiety. On a positive note, cognitive factors also mean that changing one’s focus and interpretation can reduce anxiety: techniques like Buteyko and Breatheology give control back to the person experiencing the symptoms. In sum, the link between breathing and anxiety runs through both body and mind – physiology sets the stage, and psychology determines how we dance upon it.
Disordered Breathing in Anxiety Disorders
Breathing irregularities are a hallmark of the acute anxiety response (think of someone gasping in fear), but they also play distinct roles in different anxiety disorders. Below we explore how disordered breathing manifests in some common conditions – notably panic disorder, generalized anxiety disorder (GAD), and post-traumatic stress disorder (PTSD) – and what this reveals about each condition.
Panic Disorder and Hyperventilation
Panic disorder provides a dramatic example of the breath–anxiety connection. A panic attack often seems to come “out of the blue” with a crescendo of intense fear and bodily sensations – and chief among those sensations are respiratory symptoms. Many panic attacks begin with or involve hyperventilation: patients report feeling they can’t get enough air, start breathing faster, and soon dizziness, chest pain, and tingling in the extremities join the fray. In fact, research shows that hyperventilation is present in a large proportion of panic attacks, though it may sometimes be a consequence rather than the initial cause of the attack (pubmed.ncbi.nlm.nih.gov) . The physiological effects of hyperventilation (lowered CO₂ and blood vessel constriction) can induce or amplify feelings of dyspnea (air hunger) and other sensations, which panic sufferers often find terrifying. This has led to the concept of a “respiratory subtype” of panic disorder – individuals whose panic episodes are especially tied to breathing symptoms (choking feelings, hyperventilation, etc.). Clinically, these patients often fear suffocation or choking above all else.
One of the striking findings in panic disorder is how sensitive patients are to anything that perturbs respiratory physiology. We saw earlier that inhaling concentrated CO₂ can trigger panic in most people with panic disorder, while leaving many without the disorder relatively unruffled (scientificamerican.com). Back in the 1960s and 70s, studies found that even infusing sodium lactate (which indirectly causes one to breathe faster and changes blood pH) would provoke panic attacks in patients with panic disorder but not in healthy controls, highlighting an innate vulnerability. From these observations came the influential “false suffocation alarm” hypothesis (proposed by Donald Klein in 1993), which posits that in panic disorder the brain’s suffocation-monitoring mechanism is hypersensitive and prone to false alarms (pubmed.ncbi.nlm.nih.gov). According to this theory, a slight rise in CO₂ or other signal is erroneously interpreted by the brain as if the person were suffocating, which triggers a full-blown panic – essentially a primitive reflex gone awry. While this theory has been debated, it underscores how fundamental respiratory cues are in panic. It also aligns with evolutionary logic: the panic response (surge of fear, urge to escape) may have originally evolved to deal with survival threats like asphyxiation, so it’s not surprising that misfires in this system produce intense terror.
In practice, panic disorder patients often come to fear the act of breathing itself. They may worry that “over-breathing” will cause an attack or that not breathing enough will cause them to pass out – sometimes both fears at once. This can create a tug-of-war where the person alternates between gulping air and shallow breathing. Outside of acute attacks, many have chronically altered breathing patterns; for example, some chronically hyperventilate at a low level even when anxious in a mild way, maintaining CO₂ below normal (pubmed.ncbi.nlm.nih.gov). This can leave them feeling on edge or lightheaded, essentially keeping their body in a semi-panic state. Recognizing and addressing these respiratory aspects is crucial in treatment (as we’ll discuss in the interventions section). Overall, panic disorder exemplifies a condition where disordered breathing is both a symptom and a trigger: rapid breathing can both result from panic and feed back to intensify it, creating a fearsome feedback loop.
Generalized Anxiety Disorder and Chronic Overbreathing
Generalized anxiety disorder is characterized by persistent, diffuse worry and tension rather than discrete terror episodes. The breathing patterns in GAD are therefore less acutely pronounced than in panic attacks, but over time a distinct respiratory profile can emerge. People with GAD often report symptoms like feeling breathless, tight-chested, or sighing a lot. In fact, frequent sighing or yawning can be a subtle sign of disordered breathing in GAD – essentially the body’s attempt to compensate for chronic under-ventilation or over-ventilation. Unlike panic hyperventilation, which is sudden and obvious, GAD may involve a more insidious form of dysregulated breathing. Some individuals with GAD chronically overbreathe (slightly) without realizing it, leading to continuously low CO₂ levels in the blood over the long term. This chronic hypocapnia can cause vague symptoms like light-headedness, muscle twitching, or numbness that persist and add to the person’s overall discomfort. It also overlaps with somatic symptoms of anxiety (e.g. feeling faint or jittery), potentially reinforcing worries about health or stability.
Physiological studies have noted that even at rest, anxious patients tend to have irregular breathing patterns and lower CO₂ (indicative of hyperventilation) more often than non-anxious individuals (pubmed.ncbi.nlm.nih.gov). In GAD, the worries and mental tension can translate into bodily tension, including the muscles used for breathing. Shallow “chest breathing” (using the accessory muscles in the upper chest and shoulders rather than the diaphragm) is common, which can make breathing less efficient and more effortful. This in turn might perpetuate a feeling of not getting enough air, causing more anxiety – another feedback loop. Furthermore, because GAD involves heightened vigilance, a person might over-monitor their breathing and other bodily sensations, similar to panic disorder but usually to a lesser degree of panic. For example, a GAD patient might notice “Sometimes I feel I’m not breathing right” and then become preoccupied with that feeling, leading to yet more respiratory irregularity driven by anxiety.
It’s worth noting that not everyone with GAD has overt breathing difficulties; some primarily feel muscle tension, restlessness, or other symptoms. Muscle tension, however, can be a sign of low CO₂. Researchers increasingly view “dysfunctional breathing” as a component that can co-occur with GAD. In clinical settings, breathing assessments often reveal subtle anomalies – maybe a slightly elevated breathing rate or an irregular rhythm – which, when corrected, can alleviate some of the physiological load of anxiety. Teaching GAD patients to breathe using the diaphragm and to slow their respiratory rate can sometimes reduce physical symptoms of anxiety (like heart palpitations or dizziness) and provide a greater sense of control. In summary, while GAD’s relationship with breathing is less dramatic than panic’s, chronic anxiety creates its own breathing disruptions – typically a habit of shallow, inefficient breathing with intermittent sighs – that can aggravate the overall anxiety state.
PTSD and Trauma-Related Breathing Patterns
Post-traumatic stress disorder, rooted in exposure to life-threatening or terrifying events, brings a different twist to the breathing-anxiety relationship. PTSD is marked by episodes of re-experiencing the trauma (flashbacks or nightmares), avoidance of reminders, and a pervasive state of heightened arousal (the body is persistently “on guard”). This chronic hyperarousal often manifests in the respiratory domain. Even when not in a flashback, individuals with PTSD can have an elevated resting heart rate and breathing rate, as if their body is always braced for danger. Physiologically, PTSD patients tend to show signs of autonomic dysregulation – for example, abnormally low heart rate variability, indicating an overactive sympathetic (stress) response and underactive parasympathetic calming response (va.gov). Low heart rate variability and related measures suggest that the nervous system is less flexible and more locked into a fight-or-flight state, which correlates with rapid, shallow breathing patterns.
Importantly, the chronic respiratory dysregulation in PTSD is linked with health consequences. The combination of poor sleep (due to nightmares) and sustained abnormal breathing can contribute to fatigue, cardiovascular strain, and other issues. Clinicians have observed that teaching grounding techniques that include controlled breathing can help PTSD patients manage flashbacks or anxiety surges. By focusing on slowing the breath and exhaling fully, patients engage the vagus nerve and can often diminish the intensity of a panic wave. This is not always easy – in the throes of a flashback, remembering to breathe is challenging – but with practice it becomes a tool to reconnect mind and body to the present safety. Additionally, biofeedback interventions (discussed next) have been applied to PTSD to specifically target this autonomic imbalance. In PTSD, one could say that trauma “hijacks” the breath, and part of healing is to reclaim it. Overall, PTSD illustrates how deeply breathing patterns can be altered by psychological trauma and how restoring regular, calm breathing is entwined with recovery from the anxiety of post-traumatic stress.
Breathing-Based Interventions for Anxiety
Given the profound links between respiration and anxiety, it is no surprise that breathing techniques are central in many anxiety interventions. These techniques range from age-old practices (like yoga breathing exercises) to modern biofeedback technology, but they share a common goal: to harness the breath as a tool for regulating emotional state. Here we review several major categories of breathing-based interventions – slow breathing exercises, diaphragmatic breathing, and biofeedback-assisted breathing – and the evidence behind them.
Slow, Controlled Breathing: Simply slowing down the respiratory rate is one of the most accessible strategies for calming anxiety. Often termed “paced breathing” or “slow diaphragmatic breathing,” this involves deliberately taking breaths that are longer and deeper than one’s usual anxious breathing. A typical recommendation is about 6 to 8 breaths per minute (compared to a normal ~12–20 in anxiety or at rest). Research has shown that slow breathing can effectively reduce acute anxiety and promote a state of relaxation. Physiologically, it works by enhancing parasympathetic (vagal) activity and reducing sympathetic arousal (pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov). When you exhale slowly, your heart rate naturally slows and your blood pressure can drop slightly – signals of the body settling. Over a few minutes of slow breathing, people often report feeling less tense and more in control. A recent systematic review and conceptual analysis noted that effective anxiety-reducing breath practices tend to avoid very rapid breathing and instead focus on slower, controlled patterns, with sessions lasting at least a few minutes for maximum benefit (pmc.ncbi.nlm.nih.govpmc.ncbi.nlm.nih.gov). Even extending the exhale slightly longer than the inhale (for example, inhaling for 4 seconds, exhaling for 6 seconds) is taught in some protocols to further engage the calming response. Empirical studies back this up: one scientific report found that just a session of slow breathing was associated with lowered state anxiety levels and increased feelings of calm in participants, as reflected in both self-report and physiological measures (nature.comnature.com).
Diaphragmatic (Belly) Breathing: A key aspect of effective slow-breathing is using the diaphragm – the dome-shaped muscle under the ribs – rather than just shallow chest expansion. Diaphragmatic breathing (sometimes just called “deep breathing”) encourages breathing deeply into the abdomen so that one’s belly expands on inhalation and contracts on exhalation. This method improves the efficiency of ventilation and prevents the common anxious pattern of short, shallow breaths that only fill the upper lungs. Diaphragmatic breathing has been studied for its stress-reduction benefits. A quantitative systematic review of diaphragmatic breathing exercises found consistent evidence that such practice reduces both physiological stress markers and psychological self-reported stress/anxiety (pubmed.ncbi.nlm.nih.govpubmed.ncbi.nlm.nih.gov). For example, in the studies reviewed, people who practiced belly breathing showed lower cortisol (a stress hormone) levels, lower resting heart rates and blood pressure, and reported less anxiety on questionnaires (pubmed.ncbi.nlm.nih.gov). The breathing technique essentially counteracts the hyperventilation reflex: by breathing slowly through the nose and engaging the diaphragm, CO₂ levels are maintained in a healthy range, preventing symptoms of hypocapnia (like dizziness) and thereby reducing the triggers for anxiety. Clinicians teaching diaphragmatic breathing often observe that it not only physiologically calms patients but also gives them a psychological sense of control – the act of actively modulating one’s breath can be empowering when anxiety otherwise makes one feel helpless. It is such a fundamental skill that many cognitive-behavioral therapy (CBT) programs for anxiety disorders include a component of breath retraining early on, so that patients have a tool to stabilize themselves when confronting fears.
Biofeedback and Resonance Breathing: In the modern era, technology has been added to these ancient techniques to enhance their effectiveness. Respiratory biofeedback involves providing real-time feedback to the individual about their breathing or physiological state, so they can learn to modify it. One well-established approach is heart rate variability (HRV) biofeedback, where individuals breathe at a specific rate (often around 5-7 breaths per minute, known as the “resonant” frequency) while seeing feedback (on a computer or device) of their heart rate oscillations. The goal is to maximize HRV – effectively syncing breath and heart in a healthy oscillatory pattern. Studies in populations with PTSD, for instance, have found that HRV biofeedback training can significantly reduce PTSD symptoms and improve autonomic regulation (va.gov). In one pilot study with veterans, those who received HRV biofeedback (with training in diaphragmatic breathing) showed decreased PTSD symptom scores and better heart-rate regulation, whereas a comparison group that only learned basic breathing without feedback did not achieve the same benefits (va.gov). This suggests that the feedback component – which helps users find the optimal breathing rhythm for their body – can enhance outcomes. For general anxiety and stress, HRV biofeedback has also shown positive results, improving anxiety symptoms and even cognitive function in some trials, presumably by strengthening the parasympathetic nervous system through regular practice.
Another form of biofeedback applicable to panic disorder is capnometry-assisted breathing training. Here, a device measures the CO₂ in the exhaled breath (end-tidal CO₂) and provides feedback to the user. The aim is often to increase CO₂ to normal levels (since many panic sufferers chronically hyperventilate and have low CO₂). Alicia Meuret and colleagues pioneered this approach (termed Capnometry-Assisted Respiratory Training, or CART) for panic disorder. In a controlled trial, they found that learning to raise CO₂ by breathing more slowly and shallowly – essentially reversing hyperventilation – led to significant reductions in panic attacks (blog.smu.edublog.smu.edu). Remarkably, this approach worked even when patients weren’t consciously challenging their anxious thoughts. In fact, in that study, standard cognitive therapy (which tried to change catastrophic thoughts) did not alter patients’ breathing patterns, whereas CART did normalize their CO₂ and was more successful at reducing panic symptoms (blog.smu.edu). This underscores how powerful directly targeting the physiology can be: by teaching patients how to prevent the extreme drops in CO₂ that trigger panic sensations, the therapy removed a key panic trigger. Patients often reported feeling more confident that they won’t “lose control,” because they learned that taking slower, shallower breaths (counterintuitively, not big gulps of air) prevents the onset of scary symptoms (blog.smu.edu). Breathing retraining of this sort has become a valuable tool in treating panic and hyperventilation syndrome.
Beyond these, there are many other breathing techniques and interventions – from yogic pranayama practices (like alternate-nostril breathing or “4-7-8” breathing) to mindfulness meditation focusing on the breath – all aiming to restore a harmonious breathing pattern and thereby ease anxiety. While each approach has its nuances, they share the principle of leveraging the body’s own calming mechanisms. A growing number of clinical studies and meta-analyses support the efficacy of breathing interventions. For instance, a 2023 meta-analysis of randomized trials concluded that various forms of breathwork produced significantly lower anxiety and stress levels compared to control conditions (with small-to-moderate effect sizes) (nature.comnature.com). The authors did note a need for more rigorous research, but overall the evidence aligns with centuries of anecdotal wisdom: mindful breathing can change one’s mental state. From a practical standpoint, breathing exercises are attractive because they are low-cost, drug-free, and self-directed – once a person learns the technique, they carry a portable anti-anxiety tool with them wherever they go (quite literally, in their lungs).
Doing sessions with me will incorporate Breatheology and Buteyko Method Practices. The Breatheology method will encompass vagus nerve activation, coherent breathing, breath holds, and long exhales. The Buteyko Method focuses on exclusive nasal breathing, breathing less, using the diaphragm and slowly. These methods enable me to tailor exercises to your unique situation. Breathing is likely to have different levels of impact on anxiety for different people. For some, it may all but solve it, and for others they may be able to utilize the increased self efficacy from the breathing tools to better engage in therapy of exposure to the source of stress. For many, being able to relax more will enable better recovery and soothing of the body. Even patients who are skeptical at first (“How can breathing help my severe anxiety?”) often come to value it when they notice they can abort a panic attack or steady themselves during a stressful moment by using a breathing technique. Ultimately, whether through ancient pranayama or modern biofeedback, learning to consciously control the breath offers a degree of mastery over the otherwise involuntary storms of anxiety. Book now to learn these skills with Breathcraft Lab.
Evolution of Understanding: A Historical Perspective
Our scientific understanding of the breathing–anxiety relationship has evolved tremendously over the past century. Early clinicians and researchers noticed the link well before modern experiments, but interpretations have shifted over time – from seeing disordered breathing as a cause of anxiety, to downplaying it during the cognitive revolution, and back to a nuanced view integrating body and mind. Here, we outline a brief chronology of key shifts and landmark studies that have shaped the field:
1930s – “Hyperventilation Syndrome” Identified: Clinicians observed that anxious patients often presented with symptoms like dizziness, chest pain, and faintness that were attributed to over-breathing. In 1937, Kerr and colleagues formally introduced the term “hyperventilation syndrome” to describe anxiety-related over-breathing and its symptoms (pmc.ncbi.nlm.nih.gov). This was a foundational concept suggesting that many unexplained anxiety symptoms were due to chronic hidden hyperventilation. The idea took hold that excessive breathing causes anxiety symptoms (and possibly anxiety itself), an elegant explanation that persisted for decades.
Buteyko CO₂-tolerance training (Konstantin Buteyko, USSR → modern RCTs): From Dr Buteyko’s original 1950-60s Soviet case-series—where reducing minute-ventilation and adding brief post-exhale holds reportedly cut respiratory and anxiety symptoms—to contemporary work, the method’s core finding holds: raising end-tidal CO₂ dampens the brain’s “false suffocation” alarm. A 2023 European Journal of Medical Research randomized trial in adults (n = 120) confirmed that four weeks of Buteyko drills boosted breath-hold “control-pause,” normalised CO₂, improved symptom control, and was accompanied by significant drops in self-reported anxiety scores; similar CO₂-raising protocols (CART) in panic disorder show parallel reductions in panic frequency and hyperventilation.
1960s–1970s – Biological Provocation Experiments: As biological psychiatry advanced, researchers began experimenting with induced physiological stress to trigger anxiety. Notably, Pitts and McClure (1967) found that infusing sodium lactate (which leads to changes in blood chemistry and breathing) could provoke panic attacks in individuals with anxiety disorders but rarely in healthy subjects. Similarly, studies showed that inhaling 5% CO₂ or other respiratory challenges induced panic in those with panic vulnerability. These findings pointed to an inherent physiological susceptibility in panic patients. By the late 1970s, anxiety experts like Donald Klein were speculating about built-in “suffocation alarms” misfiring. The stage was set to view some anxiety disorders as fundamentally linked to respiratory physiology.
1980s – Competing Theories: Hyperventilation vs. Cognitive Models: In the 1980s, two seemingly opposing views on panic attacks emerged. On one side, Ronald Ley and others championed the “hyperventilation theory” of panic, suggesting that panic attacks were essentially the result of sudden CO₂ drops from over-breathing (“blood, breath, and fears,” as Ley titled a 1985 paper). On the other side, David Clark’s cognitive model (1986) argued that it’s not the act of hyperventilating per se, but the misinterpretation of its sensations (“I’m dying because I feel dizzy”) that triggers panic. Empirical evidence started to complicate the picture. For example, a 1986 review by Margraf, Ehlers, and Roth found that lactate infusions didn’t consistently cause panic when psychological factors were controlled, concluding that panic is best explained by an interaction of physiological changes with cognitive appraisal and context, rather than a purely mechanical effect of hyperventilation or lactate (pubmed.ncbi.nlm.nih.gov). Meanwhile, Jack Gorman and colleagues in 1988 demonstrated that patients with panic disorder are distinctly hypersensitive to inhaled CO₂ compared to other anxious or healthy groups, supporting a respiratory vulnerability (pubmed.ncbi.nlm.nih.gov). By the end of the 1980s, the field recognized multiple pathways: hyperventilation was acknowledged as a contributor to panic but not the sole cause, and cognitive factors were integrated into the explanation of why only some people panic in response to bodily sensations.
1990s – The False Suffocation Alarm and Refined Insights: In 1993, Donald Klein formally published his “False Suffocation Alarm” hypothesis, synthesizing decades of observations (pubmed.ncbi.nlm.nih.gov). He proposed that an evolutionary suffocation-detection mechanism (perhaps involving brainstem CO₂ sensors) was oversensitive in panic disorder, causing spontaneous panics by falsely signaling “you’re suffocating” in the absence of actual danger. This hypothesis elegantly explained why CO₂, lactate, or even breath-holding could precipitate panic – these challenges all mimic aspects of suffocation. Klein’s model shifted thinking back toward biology, but with an evolutionary twist. During the 1990s, researchers also distinguished subtypes of panic (a “respiratory subtype” with prominent breathing symptoms vs. others). Another line of work in the 90s expanded the focus to other disorders: for instance, researchers explored breathing irregularities in GAD and found many GAD patients had chronic hyperventilation or sighing patterns, linking daily anxiety to breathing habits. PTSD’s profile of autonomic hyperarousal was documented, connecting trauma to chronically dysregulated respiration. By the end of the 90s, the consensus was that breathing matters across anxiety disorders, but its role is complex – sometimes a trigger, sometimes a conditioner of fear, sometimes a maintainer of physical symptoms.
2000s – Neurobiology and Integration: The turn of the millennium saw leaps in neuroscientific understanding. A groundbreaking animal study by John Wemmie and colleagues in the late 2000s showed that mice lacking acid-sensing ion channels (ASIC1a) in the brain – particularly in the amygdala – had blunted fear responses, and that CO₂ inhalation induced intense fear behaviors via these brain acid sensors (scientificamerican.com). This provided a concrete molecular mechanism tying CO₂ (and by extension breathing) to fear: panic might, at least in part, be “in the acid.” Around the same time, human brain imaging studies in panic and PTSD populations found peculiar patterns (e.g., panic patients showing abnormal brainstem and limbic activation to CO₂). There was also a resurgence of interest in the role of chronic low CO₂ (from subtle hyperventilation) in anxiety – Alicia Meuret’s work showed many panic patients had measurable hypocapnia even during everyday life, not just during attacks. Her development of capnometry-assisted therapy in the late 2000s (published in 2010) was a proof-of-concept that changing breathing could change anxiety: She demonstrated that specifically raising CO₂ levels via guided breathing led to reduction in panic symptoms, whereas traditional cognitive therapy did not affect CO₂ (blog.smu.edu). This challenged the field to reconsider earlier notions that breathing retraining was just a placebo or a distraction – instead, it appeared to directly target a core panic mechanism. Meanwhile, the polyvagal theory (Stephen Porges, 1995) gained traction, highlighting the vagus nerve’s role in emotion regulation and how slow, deep breathing might activate neural pathways of safety and social calm. By the end of the 2000s, our understanding was more integrative than ever: psychological and biological perspectives merged into biopsychosocial models of anxiety. Breathing was appreciated as both a physiological trigger and something whose perception is filtered through cognitive-emotional lenses.
2010s–2020s – New Therapeutic Applications and Ongoing Research: In the past decade, breathing techniques have become mainstream in treating anxiety and stress, and research has caught up to evaluate them rigorously. High-quality trials and meta-analyses have affirmed that breathing interventions can produce real benefits for anxiety reduction (nature.comnature.com). Breathing practices from Eastern traditions (like yoga pranayama) entered Western clinical science, leading to studies on techniques such as alternate-nostril breathing or the “4-7-8” breath for anxiety relief. Heart-rate variability biofeedback emerged as a promising therapy for PTSD, generalized anxiety, and even depression, with multiple studies showing it improves symptoms by training respiratory-autonomic control (va.govva.gov). Technological advancements also made at-home practice easier (smartphone apps that guide breathing or provide feedback became popular). The late 2010s saw an explosion of public interest in “breathwork,” as evidenced by best-selling books and media coverage, which in turn spurred more scientific inquiry into how exactly different breathing patterns impact the brain. Neuroscientists began examining, for instance, how slow breathing influences brain oscillations and connectivity. COVID-19 (2020s) further thrust breathing into the spotlight – both because the virus attacks respiratory function and because the pandemic’s stress led many to seek breathing-based stress reduction. The result is a surge of interdisciplinary interest: pulmonologists, psychologists, and neurologists collaborating to map out the precise links between breath and emotional states. While many questions remain (e.g., identifying which breathing technique is optimal for which individual, understanding long-term effects), the trajectory is clear: from a once simplistic hyperventilation theory, we now have a rich, multifaceted understanding of the breath–anxiety connection, encompassing cellular sensors, brain circuits, behavior, and therapeutic techniques.
Conclusion
Breathing is unique among bodily functions in that it lies at the crossroads of the conscious and unconscious, the voluntary and involuntary. This duality may be why it plays such a pivotal role in anxiety. We don’t usually notice our breathing, until something goes awry, as it often does in moments of fear. Then, the quick breaths, the feeling of air hunger, or the tight chest become front-and-center in our awareness, signaling that something is not right. What science has revealed is that this “not right” can be a false alarm as much as a true one: our bodies can cry suffocation in the absence of real danger, and our minds can amplify that cry into panic. The relationship between breathing and anxiety is thus a feedback loop, with physiology and psychology in constant dialogue.
On the bright side, this interconnection means we have a powerful entry point for intervention: by modulating the breath, we can modulate anxiety. The research reviewed shows that techniques as simple as slowing one’s breathing or biofeedback can reduce anxiety symptoms, sometimes dramatically. These findings validate the experiences of many people who have long used practices like yoga breathing or meditation to manage stress. They also offer tangible strategies for clinicians and individuals dealing with anxiety disorders sometimes as cures and sometimes as complementary tools alongside therapy or medication. Importantly, breathing techniques empower patients to actively participate in their own calming, fostering a sense of control that anxiety often steals away.
For anyone who has felt the clutch of anxiety and noticed their breath feel tense, this research offers validation you’re not abnormal for feeling like you can’t breathe, nor are breathing exercises “silly” tricks. They tap into real physiological mechanisms. And for the scientifically curious, the breath–anxiety link is a fascinating example of how evolution equipped us with mechanisms to survive threats (like low oxygen) that sometimes misfire in modern life, but also how we can consciously engage those mechanisms to find calm. In conclusion, the dance between breath and anxiety is intricate and deeply rooted in our biology, but by understanding its steps, we can learn to lead, not be led by, the rhythm of our own breathing (pmc.ncbi.nlm.nih.govscientificamerican.com).
If you are ready to learn tailored breathing strategies book your free 15 minute consultation now with Breathcraft Lab, or, email us for our next group course.